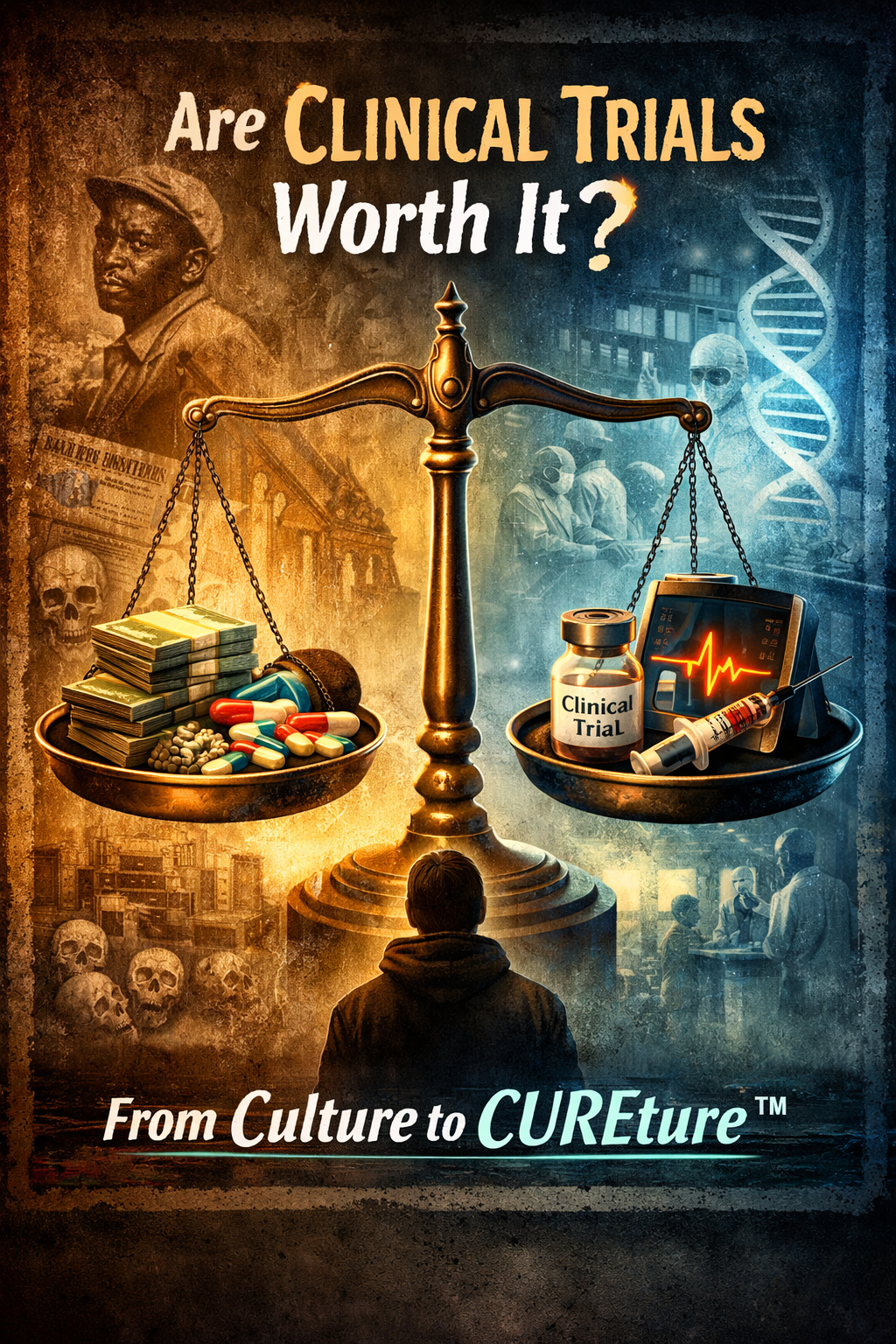
Are Clinical Trials Worth It?
Medical Mistrust is Justified.
“No one of any race should ask evil if it can be trusted. You might enjoy a few conveniences and even feel included for a short while, but in the long run, you are being exploited or marinated for consumption. You should never trust man, that confidence should be extended to God; instead, engage people with clear knowledge of what you are giving up while you weigh whether what you are giving is worth what you’re getting.”
— Pastor Ada Hailey (Mom)
Many have heard medical professionals advocate for the importance of clinical trials. Patients are routinely encouraged to participate when eligible and able. Yet this messaging is often underinformed and incomplete. It frequently omits the historical realities of medical mistreatment, misdiagnosis, and structural abuse, particularly among certain communities and socioeconomic groups.
This omission matters.
While it is true that clinical trials are essential to medical progress, it is also true that they operate within economic and institutional systems. Clinical research generates revenue, prestige, intellectual property, and commercial pipelines. Failing to acknowledge this reality contributes directly to medical mistrust, mistrust that is often portrayed as irrational when, in fact, it is historically and empirically grounded.
Patients today are not only researching treatment options. They are researching systems. They are learning to follow the money: who funds studies, who profits from discoveries, how procedures are billed, and where incentives truly lie. When patients discover that benefits may accrue disproportionately to institutions rather than communities, skepticism is not only understandable, it is rational.
That skepticism does not mean clinical trials lack value.
So, let us ask the more honest question: under what conditions do clinical trials become worth it for patients?
Assuming access to a trusted, independent advocate—someone whose sole priority is maximizing your outcome based on your values—two reasons remain compelling.
The first is altruism. Despite corruption, greed, and institutional failures, many decent, intelligent, non-corrupt scientists and clinicians are genuinely working to reduce suffering and save lives. Participation in clinical trials has repeatedly advanced human health, even when systems surrounding that work have fallen short of ethical ideals.
The second reason is hope—not naïve hope, but informed possibility.
Advancements in medical science follow a clear long-term upward trajectory, yet the timing and nature of major breakthroughs remain inherently unpredictable. Progress tends to occur in irregular bursts, emerging from complex interactions among scientific insight, technology, and resource availability. Sustained financial investment increases the likelihood of discovery, but never its timing.
This means something important:
The clinical trial that extends a life today may create the window needed to benefit from a breakthrough that emerges tomorrow.
History shows this has happened before.
A cure is never promised. But possibility exists.
Imagine living long enough on a trial for a discovery—initiated years earlier—to finally materialize. Imagine being the life extended just enough to benefit from progress already underway. Would that matter then?
Consider the possibilities while reading about this work:
https://www.cnio.es/en/news/the-group-led-by-barbacid-at-cnio-completely-eliminates-pancreatic-tumours-in-mice-with-no-resistance-developing/
I invite you to sit with the tension, not blind trust, not blanket rejection, but informed engagement. Clinical trials are neither saints nor villains. They are tools. And tools must be handled with Awareness, Decision, and Commitment for those most vulnerable.
If you’re considering a study and want someone you can trust, I am here for you.